Percutaneous Diagnosis of Chest, Lung Problems
You’ve been told you need a percutaneous procedure to diagnose a problem in your chest or lung. This procedure lets the healthcare provider remove tissue or fluid (biopsy) from the chest or lung. For these procedures, the skin of the chest is cleaned and numbed. Then, a needle is passed through the skin.
Fine-needle aspiration biopsy
Fine-needle aspiration biopsy is a procedure used to take a lung tissue sample (a tissue biopsy). The tissue sample is taken from a nodule, abnormal tissue, tumor, or lung mass. First, a CT scan or ultrasound is done. This helps the healthcare provider find the area. Then, a thin needle is passed through the skin of the chest into the nodule, abnormal tissue, tumor, or lung mass. Another CT scan or a chest X-ray is taken to be sure the needle is placed correctly. Once the needle is in place, a small amount of lung tissue is drawn (aspirated) into the needle. The lung tissue sample is then sent for testing.
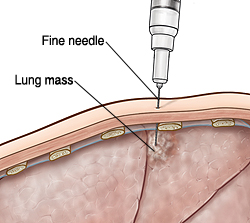 |
| With FNA, a thin needle is used to take a tissue sample from a mass. |
Thoracentesis
Thoracentesis drains abnormal fluid buildup between the lungs and chest wall (the pleural space). For the procedure, after the skin is numbed with medicine, a needle is put through the skin of the chest into the pleural space. Fluid is then drawn into the needle and later tested for cancer and other problems.
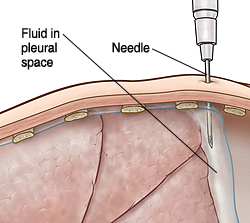 |
| Thoracentesis is used to remove fluid from the pleural space. |
Getting ready for the procedure
Before your procedure, do the following:
-
Follow any directions you are given for not eating and drinking before the procedure.
-
Tell your healthcare provider about any medicines you take. This includes over-the-counter or prescription medicines, vitamins, herbs, or other supplements. You may need to stop taking certain medicines before the procedure, especially aspirin, warfarin, ibuprofen, or other blood thinners.
-
Talk with your provider about any allergies, recent illnesses, and health problems you may have.
-
Tell your provider if you're pregnant or think you could be pregnant.
-
Talk to your provider about any questions or concerns you have.
During the procedure
You will receive local anesthesia (numbing medicine) to keep you from feeling pain. The area where the needle goes in is numbed. If your provider uses ultrasound to guide the needle, you'll also have cool gel placed on your skin in the area to help the ultrasound probe move around. Medicine to help you relax (sedation) may also be given through an IV (intravenous) line.
After the procedure
You may have some pain after the procedure. But in most cases, it's not severe. You'll be given medicine to help ease any pain. You can go home after you recover from anesthesia, often the same day as the procedure. If you received sedation, an adult family member or friend will need to drive you home. If a tube was placed in your chest to drain fluid and was left in, you will stay in the hospital for at least 1 day or more. Your healthcare provider will tell you more.
Risks and possible complications
All procedures have some risk. Possible risks of this procedure include:
-
Bleeding or coughing up blood
-
Collapsed lung (pneumothorax)
-
Infection
-
Injury to other structures in the chest
-
Chest pain
-
Other complications as explained by your provider
When to call your healthcare provider
Call your provider if any of these occur: