When Your Child Has Pharyngitis or Tonsillitis
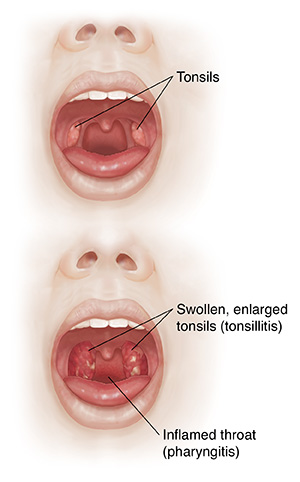
Your child’s throat feels sore. This is likely because of redness and swelling (inflammation) of the throat. Two areas of the throat are most often affected. These are the pharynx and tonsils. Inflammation of the pharynx (pharyngitis) and inflammation of the tonsils (tonsillitis) are very common in children. This sheet tells you what you can do to ease your child’s throat pain.
What causes pharyngitis or tonsillitis?
Most commonly, pharyngitis and tonsillitis are caused by a viral or bacterial infection.
What are the symptoms of pharyngitis or tonsillitis?
The main symptom of both conditions is a sore throat. Your child may also have a fever, redness or swelling of the throat, and trouble swallowing. You may feel lumps in the neck.
How is pharyngitis or tonsillitis diagnosed?
The healthcare provider will look at your child’s throat. The healthcare provider might wipe (swab) your child’s throat. This swab will be tested for the bacteria that causes an infection called strep throat. If needed, a blood test can be done to check for a viral infection such as mononucleosis.
How is pharyngitis or tonsillitis treated?
If your child’s sore throat is caused by a bacterial infection, the healthcare provider may prescribe antibiotics. Otherwise, you can treat your child’s sore throat at home. To do this:
-
Give your child acetaminophen or ibuprofen to ease the pain. Don't use ibuprofen in children younger than 6 months of age or in children who are dehydrated or vomiting all of the time. Ask your child's healthcare provider about how much and when to give the medicine.
-
Don’t give your child aspirin to relieve a fever. Using aspirin to treat a fever in children could cause a serious condition called Reye syndrome.
-
Give your child cool liquids to drink.
-
Have your child gargle with warm saltwater if it helps relieve pain. This is typically recommended for children over the age of 6. Recipes usually suggest ¼ to ½ teaspoon of salt in a cup (8 ounces) of warm water.
-
Try an over-the-counter throat numbing spray.
Always talk with your child's healthcare provider before giving your child any over-the-counter medicines, especially if it's the first time your child will be taking the medicine.
What are the long-term concerns?
If your child has frequent sore throats, take them to see a healthcare provider. Removing the tonsils may help relieve your child’s recurring problems.
When to call your child's healthcare provider
Call your child’s healthcare provider right away if your otherwise healthy child has any of the following:
-
Fever (see Fever and children, below)
-
Sore throat pain that persists for 2 to 3 days
-
Sore throat with fever, headache, stomachache, or rash
-
Trouble turning or straightening the head
Call 911
If your child has any of these symptoms, call 911 right away:
-
Problems swallowing or drooling
-
Trouble breathing or needing to lean forward to breathe
-
Problems opening mouth fully
-
Trouble speaking
-
Skin that is blue, purple, or gray in color
-
Loss of consciousness or problems waking
-
Feeling faint or dizzy
-
Shortness of breath with a fast heartbeat
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older