Continuous Epidural Infusion for Pain Relief
Continuous epidural infusion is a way to give pain medicine. The medicine is sent to the spinal cord and nerves. This is done through a soft tube (catheter). The catheter is put in the spine into the epidural space. This space surrounds your spinal cord. The tube is connected to a small device that sends pain medicine. Pain signals in part of your body are then blocked.
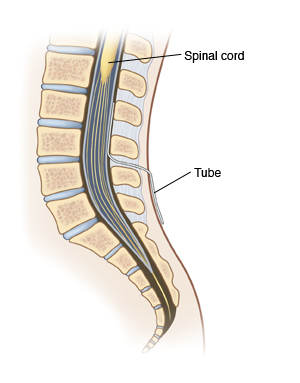 |
| For a continuous epidural, medicine is sent through a tube into the space outside of your spinal cord. |
Why an epidural is used
Continuous epidural infusion is often used to treat pain after surgery. It's often put into place before a surgery. It can stay in place for the first few days of recovery. An epidural is also used when it may give better pain relief than pain medicines taken by mouth (oral) or put into a vein.
How an epidural works
Pain signals from nerves in the affected part of your body travel up the spinal cord to your brain. An epidural blocks nerve signals from traveling up the spinal cord. This keeps the signals from reaching your brain. And this stops you from feeling the pain. A thin, soft tube (catheter) is used. It's put through the skin of your back into the part of the spinal canal around the spinal cord called the epidural space. Medicine is then sent through the tube. It blocks nerves below the point where the tube is inserted. The medicines either reduce pain or block most feeling.
The epidural insertion
The epidural may be put in before surgery. Or it may be put in just after surgery. If you are awake for the insertion, you may be asked to lie on your side. You will pull your knees up to your stomach. Or you may be asked to sit on the side of your bed. You will then lean over. An area of skin on your back is cleaned and numbed with anesthetic. A special needle is put into your back. The provider then puts a catheter inside the needle and into the epidural space. The needle is removed, and the catheter remains in place. A small machine pumps pain medicine through the tube. The pump is programmed and adjusted by the anesthesiologist. In some cases, you will be shown how to give yourself medicine as needed.
When the epidural is in place
-
You may be able to move around and walk with the epidural in place. Ask your healthcare provider before trying to walk with it in place.
-
The medicine may make you unable to empty your bladder. If this happens, the amount of medicine may be adjusted. Or a tube is placed into your bladder to drain it.
-
If you have certain symptoms, your medicine may be adjusted. Tell your healthcare provider if you:
-
The epidural can be left in place for several days. It will be removed before you go home.
Risks and possible complications of continuous epidural
All procedures have risks. The risks of this procedure include:
Your healthcare provider or nurse will watch for these problems while the epidural is in place.